The Quest To Stop Cancer From Coming Back
How physicians, researchers and advocates are working towards this goal for patients
Originally published on Bristol Myers Squibb News & Perspectives
In his 15 years as a lung cancer specialist, Professor Nicolas Girard, MD, PhD, of the Curie-Montsouris Thorax Institute has seen – and helped advance – dramatic changes in how patients with this disease are treated. Yet despite this progress, lung cancer remains the leading cause of cancer deaths globally, and even patients who are diagnosed early often experience recurrence.
“Patients with lung cancer who are eligible for resection undergo surgical treatment with a curative intent, meaning the aim is to avoid any event related to cancer after surgery,” said Professor Girard. “Unfortunately, given the aggressiveness of the disease, many patients eventually experience recurrence.”
Some patients receive chemotherapy before or after surgery with the goal of reducing the likelihood of the cancer’s return, but the evidence to support this treatment approach remains limited. To better protect patients with lung cancer against disease recurrence, additional treatment options are needed urgently.
Danielle Hicks, chief patient officer at the GO2 Foundation for Lung Cancer, has experienced this unmet need firsthand. When her mother was diagnosed with stage 3b lung cancer in 2003, she was initially told there were no options at the time but to go home.
“Walking side-by-side with my mother though her treatment process, I learned that navigating treatment options can be an overwhelming experience,” said Hicks.
Fortunately, Hicks’ mother defied the odds and is still alive today. The two went on to use their experience to educate and advocate for people living with lung cancer.
“Many people don’t understand the difference between an early-stage or metastatic diagnosis – they believe that cancer is treated the same way,” Hicks said. “Anytime someone hears they have cancer, they very rarely hear what is said next. It is terrifying regardless of the stage of the disease.”
Disrupting the course of cancer with immunotherapy
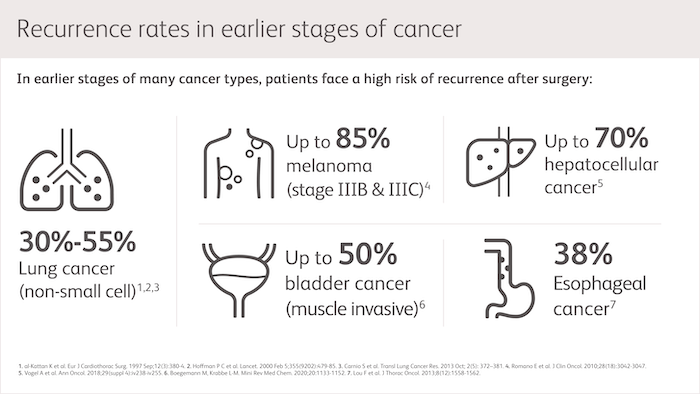
Though earlier-stage cancers generally have better prognoses, recurrence often marks the transition to incurable disease and represents a life-altering event for patients. That raises an important question for researchers: what can be done in addition to surgery, to reduce the chance of recurrence?
Mark Rutstein, MD, vice president of Oncology Development at Bristol Myers Squibb, is one of the many researchers looking to tackle this problem.
One strategy that Rutstein and his team are investigating is the use of immunotherapy, which works with the body’s immune system to help address cancer. Immunotherapy research started in the metastatic setting, where there was the most immediate need to extend lives.
Now, Rutstein hopes to build on this progress by exploring the potential benefits of bringing immunotherapy into the neoadjuvant (before surgery), adjuvant (after surgery) and peri-operative (both before and after surgery) settings. The science of cancer and the immune system supports this effort.
“In earlier stages of cancer, patients’ immune systems may be more intact, potentially making them better candidates for immunotherapy,” said Rutstein. “Additionally, tumor burden is often lower post-surgery, enabling the possibility for either a long-term clinical benefit or cure with systemic treatment.”
This insight is important to physicians like Professor Girard, who is eager to help his patients achieve better outcomes.
“The ultimate goal of treatment, whether treatment is given in the neoadjuvant, adjuvant or peri-operative setting, is to prevent recurrence. In other words, our aim is to improve survival rates and long-term outcomes for patients,” he said.
In the past few years, there have been noteworthy advances in research evaluating immunotherapy in earlier stages of cancer. The next step? According to Professor Girard, further studies should prioritize identifying which patients may respond best to immunotherapy in earlier disease settings by analyzing biomarkers and their interactions with the immune system.
"When the immune system is not yet exhausted, as we may see in metastatic disease, we may use immunotherapy before or after surgery to stimulate the interaction between the immune system and cancer cells."
–Nicolas Girard, MD, PhD, professor of respiratory medicine and head of Curie-Montsouris Thorax Institute, Curie Institute
Improving long-term patient outcomes
To Hicks, making progress in earlier-stage cancer intervention matters on both a personal and professional level. She has spent the last fifteen years working with people diagnosed with different stages and types of lung cancer and continues to advocate for them every day.
“I made a conscious choice a long time ago to stand next to these people – to help educate and empower them on their disease, and to help them find hope in their tomorrows,” said Hicks.
Rutstein, too, is hopeful that continued research will lead to improved long-term outcomes and looks forward to seeing this goal become a reality for patients and their families.
“It is remarkable to see how far we’ve come with researching immunotherapy in earlier stages of cancer – to see its potential to prevent disease recurrence and interrupt the trajectory of the disease,” he said.
“Having lost family and friends to cancer, it gives me great pride to be part of the process of studying immunotherapy in earlier disease settings, knowing that we have the potential to impact many patients in meaningful way.”